The Testicles
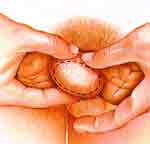
The total exam takes only three minutes. Start
by holding your scrotum in the palms of your hands.
Then feel one testicle. Apply a small amount of
pressure. Slowly roll it between your fingers.
Try to find hard, painless lumps.
|
 |
The Epididymis
Now, examine your epididymis. This comma-shaped
cord is found behind your testicles. It's job
is to store and transport sperm. Tender when touched,
it is the location of most non-cancerous problems.
|
 |
The Vas
Continue by examining the vas, the sperm-carrying
tube that runs up from your epididymis. Normally,
the vas feels like a firm, movable smooth tube.
Now, repeat the exam on the other side.
|
 |
 |
|
 |
| Seminomas-
About half of all the cancers of the testicle
are seminomas, or tumors. They are generally found
at an early stage, before they have spread. Males
with an early seminoma have close to a 100% cure
rate if treated with surgery and radiation. |
|
Nonseminomas-
These are difficult to cure because they are not
as responsive to radiation treatments as are seminomas.
There are several types of nonseminomas, but the
recommended treatment is almost always the same:
Surgical removal of the cancerous testicle. Such
a procedure is necessary because nonseminomas
are very dangerous. |
Physical Examination:
The first step in diagnosing any problem with
the scrotum or testicles is a thorough physical
examination by a physician. For further evaluation,
referral to a urologist or other specialist may
be necessary.
|
|
Ultrasonography
This technique uses sound waves directed towards
the testicles. Echo waves from the sound probe
are analyzed for patterns that suggest abnormal
tissue growth. |
Computerized Axial Tomography (CAT Scan)
This is a special computerized X-ray study
of the body. It helps the physician determine
the existence and location of tumors and other
cancerous masses in the body.
|
|
Transillumination
In this method, a very intense beam of light
is passed through the thin skin of the scrotal
sac. Abnormalities like solid masses within the
scrotum are detectable because they will not allow
light to pass through.
|
Lymphangiography
This procedure involves X-rays of the lymph
system following injection with a special dye.
Using this technique, a physician can detect
blockages in the lymph system that may suggest
cancer.
|
|
Aspiration
With aspiration, a syringe and needle are used
to withdraw fluid from any cyst or tumor. The
removed sample of liquid is then examined in the
laboratory.
|
Intravenous Pyelography (IVP)
IVP involves special dyes and X-ray studies
of the kidneys, bladder, and other structures
of the urinary system. It allows the physician
to check for blockages and other abnormalities
of the urinary tract.
|
|
Biopsy
Biopsy is a procedure in which a very small
piece of suspicious tissue- like a tumor or cyst
- is removed and examined in the laboratory.
|
Magnetic Resonance Imaging (MRI)
Also known as Nuclear Magnetic Resonance (NMR),
this procedure uses magnetization and radio frequencies
to produce detailed images of internal body structures.
The MRI is used for the same purposes as a CAT
scan. |
|
Orchiectomy (Orchectomy; Orchidectomy)
This procedure is the surgical removal of
a testicle. The removed organ is examined in
the
laboratory to confirm the presence of cancer.
An artificial testicle may be used to replace
the one that was removed.
|